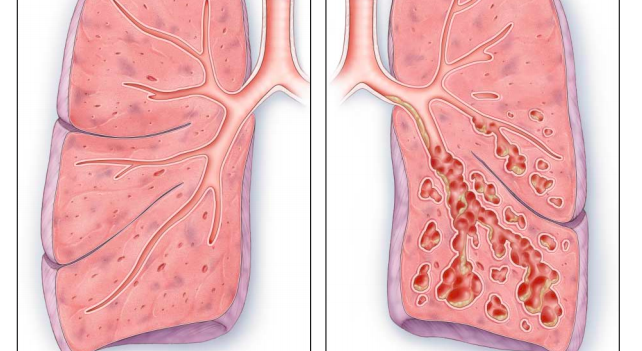
Bronchiectasis is an obstructive lung disease that results from the presence of chronic inflammatory secretions and microbes leading to the permanent dilation and distortion of airway walls, as well as recurrent infection .
 |
| Bronchiectasis |
MECHANISM OF INJURY/ PATHOLOGICAL PROCESS
Bronchiectasis is chronic irreversible dilation of the bronchi on the lungs. It follows a severe lung infection or aspiration. It is more common in conditions such as Cystic Fibrosis, Rheumatoid Arthritis, Immunodeficiency, Young’s syndrome and Allergic Bronchopulmonary Aspergillosis, and after chilhoos diseases such as whooping cough, TB and measles.
CLINICALLY RELEVANT ANATOMY
ANATOMY OF LUNG
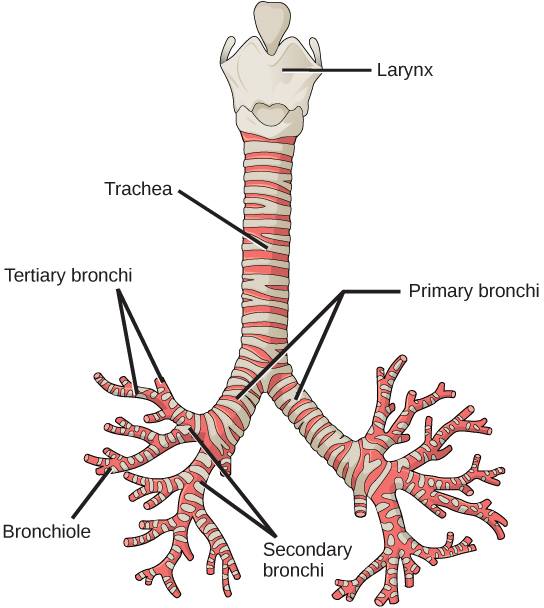
Bronchiectasis involves inflammation of the airway walls, specifically the bronchial walls . The airway walls are the ‘tubes’ that run from the mouth and nose and travel to the lung. The main area that is affected in bronchiectasis is the bronchi . The trachea bifurcates into the right and left main bronchi, which then further divide into secondary bronchi; one for each lobe of the lung . They then divide into tertiary bronchi; one for each bronchopulmonary segment .
The cilia are also damaged in bronchiectasis. Cilia line the airway and are attached to the epithelium. They are hair-like with tiny hooks on the tip to grab the mucous and help move the mucous up to the throat .
EPIDEMIOLOGY
It is underestimated in prevalence, incidence, and morbidity because symptoms are often ascribed to smoking. A study by Hill found that one in 1000 Britans have bronchiectasis, with associated deaths increasing at a rate of approximately 3% per year in England and Wales . Though the overall mortality rate is increasing in these countries, rates in older groups are rising whereas rates in younger groups are falling . A disproportionate amount of cases found in developing countries and in Aboriginal populations in affluent communities . In some populations, an improvement in socio-economic status, housing, and education can improve overall health and reduce the incidence of respiratory infection and development of bronchiectasis .
AETIOLOGY
The cause is unknown for 50% of cases, but it has been linked to inflammatory bowel disease, rheumatoid arthritis, and in 29-50% of patients, COPD .There are several associated conditions with bronchiectasis including; cystic fibrosis, primary ciliary dyskinesia, lung tuberculosis, allergic bronchopulmonary aspergilosis, rheumatoid diseases, symptomatic lupus erythematosus, immune deficiency, severe childhood respiratory infection and exposure to foreign body or corrosive substance . It has also been linked to an x1-antitrypsin deficiency . Bronchiectasis tends to predispose patients to acquired and congenital lung infections.
PATHOPHYSIOLOGY
Currently, a high-resolution CT scan is the gold standard for diagnosis of bronchiectasis. Parallel tramlines and ring shadows may be present on the scan, indicating thickened airway walls and dilated airways, respectively. There may also be ‘glove finger shadows’, which are finger –like projections that represent the dilated bronchi filled with solidified secretion.
Spirometry will simply identify if there is an airway obstruction, but this can be indicative of many other diseases.
Microbiology can also be used to identify the bacteria present during an exacerbation . A sputum sample is sent off and the results are returned with the incidence of bacterial colonization measured .
CLINICAL MENIFESTATION
As delicate cilia are often damaged due to the presence of thick mucus, the voluminous quantities of sputum formed cannot be efficiently cleared. These secretions will lead to the production of wheezes, coarse crackles and squeaks on auscultation. Often times, patients will also present with muscular dysfunction due to inflammation, gas exchange abnormalities, inactivity, malnutrition, hypoxia and medications. Dyspnoea on exertion seems to be a major clinical manifestation as it is experienced by three out of four patients. Other physical manifestations include chest pain, snoring, finger clubbing, fatigue, persistent cough, recurrent infection, and loss of appetite. Stress incontinence can also be a result of excess coughing. Bronchiectasis tends to also have psychological manifestations, such as anxiety, depression, reduced confidence, altered relationships and time off work.
Exacerbations can occur several times a year and are identified by four or more of the following signs and/or symptoms: change in sputum, increased dyspnoea, increased cough, fever of greater than 38°, increased wheeze, decreased exercise tolerance, fatigue, lethargy, and radiographic signs of a new infection.
DIAGNOSIS

ABNORMAL AIRWAY DILATION OF LUNG
Currently, a high-resolution CT scan is the gold standard for diagnosis of bronchiectasis . Parallel tramlines and ring shadows may be present on the scan, indicating thickened airway walls and dilated airways, respectively. There may also be ‘glove finger shadows’, which are finger –like projections that represent the dilated bronchi filled with solidified secretions.
Spirometry will simply identify if there is an airway obstruction, but this can be indicative of many other diseases.
Microbiology can also be used to identify the bacteria present during an exacerbation . A sputum sample is sent off and the results are returned with the incidence of bacterial colonization measured .
PHYSIOTHERAPY AND OTHER MANAGEMENT
Treatment for bronchiectasis aims to:
- Decrease symptoms (such as cough and fatigue)
- Decrease frequency and severity of exacerbations
- Decrease hospital admissions
- Improve quality of life
- Improve exercise tolerance
- Maintain or improve lung function
- Prolong survival
- Defining patient specific treatment goals.
An important part of a management plan is to define patient specific treatment goals. This may include:
Identifying:
- Symptoms type and duration
- Sputum volume and characteristics (colour thickness, smell, ease of clearance, presence of blood)
- Frequency of exacerbations (previous hospitalisations and antibiotics)
- Responses (and adverse effects) to previous treatments (antibiotics)
- Haemoptysis volume and frequenc
- Identifying co-morbidities that can contribute to bronchiectasis symptoms
- Sinusitis
- Gastro Oesophageal Reflux (GORD)
- Asthma / ABPA
- COPD and chronic bronchitis
- Identify and promoting self-care activities
- Exercise
- Airway clearance
- Symptom monitoring
The overall treatment plan aims to minimise symptoms and exacerbations with the long-term objective of maintaining lung function.
Physiotherapy is an essential part of the treatment for bronchiectasis. Because of the infection in the lung, secretions build up. Being able to cough the secretions up is important as this drains the chest of infected mucus.
All patients with bronchiectasis will have time with a physiotherapist, who will teach the techniques for getting the mucus up and draining the secretions from the lungs. The three methods illustrated in the video are the commonest forms of physiotherapy.
The first two, Acapalla and Active cycle of breathing can be taught by a physiotherapist. This will enable the you to perform these chest clearance methods on your own helping to keep you as healthy and infection free as possible.
The Active Cycle of Breathing Techniques (ACBT) is an active breathing technique performed by the patient to help clear their sputum the lungs. The ACBT is a group of techniques which use breathing exercises to improve the effectiveness of a cough, loosen and clear secretions and improve ventilation.
ACBT consists of three main phases:

ACBT TEQNIC
1.Breathing Control
2.Deep Breathing Exercises or thoracic expansion exercises
3.Huffing OR Forced Expiratory Technique (F.E.T)
Additionally, a manual technique (MT) or positive pressure can be added if and when indicated, to create a more complex cycle to help improve removal of secretions on the lungs.
1. BREATHING CONTROL
Breathing control is used to relax the airways and relieve the symptoms of wheezing and tightness which normally occur after coughing or breathlesnes. Breathing should be performed gently through the nose using as little effort as possible. If this is not possible then breathing should be done by mouth. If it is necessary to breathe out through the mouth this should be done with ‘pursed lips breathing’. While performing this technique it is important to encourage the patient use it as an opportunity to reduce any tension they may have, Encouraging the patient to close their eyes while performing Breath Control can also be beneficial in helping to promote relaxation. It is very important to use Breathing Control in between the more active exercises of ACBT as it allows for relaxation of the airways. Breathing Control can also help you when you are short of breath or feeling fearful, anxious or in a panic. The length of time spent performing Breathing Control will vary depending on how breathless patient feels.
When using this technique with a patient as part of the ACBT the patient should be instructed to usually 6 breaths. Instructions to patient: Rest one hand on your stomach and keep your shoulders relaxed to drop down. Feel your stomach rise as you breathe in and fall when you breathe out.
2. DEEP BREATHING EXERCISE
Deep breathing is used to get air behind the sputum stuck in small airways:
Relax your upper chest.
Breathe in slowly and deeply.
Breathe out gently until your lungs are empty – don’t force the air out.
Repeat 3 – 4 times, if the patient feels light headed then it is important that they revert back to the Breathing Control portion of the cycle.
At the end of the breath in, hold the air in your lungs for 3 seconds (this is known as an inspiratory hold).
Deep breathing/thoracic expansion exercises recruit the collateral ventilatory system assisting, the movement of air distal to mucus plugs in the peripheral airways.
Deep breaths to utilise collateral channels and get air behind sputum to mobilise it towards larger airways and towards the mouth. Instructions to patient:
Relax your shoulders.
Place both hands on either side of ribs.
Breathe in deeply feeling as your ribs expand.
Breathe out gently as far as you can until your lungs feel empty.
Deep breathing/thoracic expansion is usually repeated 4 times.
3. HUFFING or FET
The FET is an integral part of the ACBT described by Pryor and Webber .
A huff is exhaling through an open mouth and throat instead of coughing.Huffing moves sputum from the small airways to the larger airways, from where they are removed by coughing. Coughing alone does not remove sputum from small airways.
Take a small-medium sized breath in
Squeeze the breath out by contracting your tummy muscles and keep your mouth and throat open to perform a huff. This small-medium sized huff helps with the removal of sputum in the lower reaches of the lungs.
To remove sputum in the higher portions of the lungs take a large breath in.
Squeeze the air out as before to perform a huff.
Cough and expectorate any sputum. If no sputum is produced with 1 or 2 coughs, try to stop coughing by encouraging the patient to use Breathing Control, the main technique used in between the more active stages of the as ACBT.
Allow your breathing to settle with breathing control and then repeat the cycle until your chest feels clear.
Small long huffs move sputum from low down into chest whereas big short huffs moves sputum from higher up into chest, so use this huff when it feels ready to come out, but not before; huffs work via dynamic compression.



0Comments