Lumbar Spondylosis can be described as all degenerative conditions affecting the disks, vertebral bodies, and associated joints of the lumbar vertebrae.
Spondylosis encompasses numerous associated pathologies including spinal stenosis, degenerative spondylolisthesis, osteoarthritis and many others. It also captures effects of aging, trauma and just the daily use of the intervertebral discs, the vertebrae, and the associated joints.
Pathology of Lumbar Spondylosis:
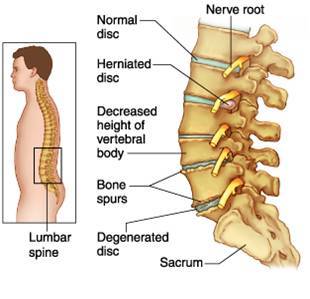
The degenerative effects of ageing can cause the fibers of the discs to weaken, causing wear and tear. Constant wear and tear and injury to the joints of the vertebrae causes inflammation in the joints. Degeneration of the discs leads to the formation of mineral deposits within the discs. The water content of the center of the disc decreases with age and as a result the discs become hard, stiff, and decreased in size. This, in turn, results in strain on all the surrounding joints and tissues, causing the sensation of stiffness. With less water in the center of the discs, they have decreased shock absorbing qualities. An increased risk of disc herniation also results, which is when the disc abnormally protrudes from its normal position.
 |
| Lumbar Spondylosis |
LUMABAR SPONDYLOSIS
Each vertebral body contains four joints that act as hinges. These hinges are known as facet joints or zygapophyseal joints. The job of the facet joins is to allow the spinal column to flex, extend, and rotate. The bones of the facet joints are covered with cartilage (a type of flexible tissue) known as end plates. The job of the end plates is to attach the disks to the vertebrae and to supply nutrients to the disc. When the facet joints degenerate, the size of the end plates can decrease and stiffen. Movement can stimulate pain fibers in the facet joints and annulus fibrosis. Furthermore, the vertebral bone underneath the end plates can become thick and hard.
Degenerative disease can cause ligaments to lose their strength. A ligament is a tough band of tissue that attaches to joint bones. In the spine, ligaments connect spinal structures such as vertebrae and prevent them from moving too much. In degenerative spondylosis, one of the main ligaments (known as the ligamentum flavum) can thicken or buckle, making it weaken.
Knobby, abnormal bone growths (known as bone spurs or osteophytes) can form in the vertebrae. These changes can also cause osteoarthritis. Osteoarthritis is a disease of the joints that is made worse by stress. In more severe cases, these bones spurs can compress nerves coming out of the spinal cord and/or decreased blood supply to the vertebrae. Areas of the body supplied by these nerves may become painful or develop loss of sensation and function.
Risk factors for developing lumbar spondylosis:
• Age: As a person ages the healing ability of the body decreases and developing arthritis at that time can make the disease progress much faster. Persons over 40 years of age are more prone to developing lumbar spondylosis.
• Obesity: Overweight puts excess load on the joints as the lumbar region carries most of the body’s weight, making a person prone to lumbar spondylosis.
• Sitting for prolonged periods: Sitting in one position for prolonged time which puts pressure on the lumbar vertebrae.
• Prior injury: Trauma makes a person more susceptible to developing lumbar spondylosis.
• Heredity or Family history.
Lumbar Spondylosis : Symptomes :
Patients suffering lumbar spondylosis also have neurologic claudication, which includes: lower back pain, leg pain, numbness when standing and walking. These symptoms improve in sitting and supine positioning.
Other characteristics:
• Pedicle anteroposterior dimension, obliquity and the relative interarticular process-interpedicle dimensions are important osteological determinants of the presence and size of lateral recesses at different vertebral lumbar levels.• The osteo-ligamentous nerve root canals and their terminal intervertebral canals show significant normal narrowing at the level of the opposed intervertebral discs and facet joint capsules. This narrowing causes a “grain” appearance in the normal nerve root canals and of the appearance of long-necked gourds in the osteo-ligamentous intervertebral canals. The narrowing of the disc intervertebral is an important cause of many of the degenerative changes in the lumbar spine.
Differential Diagnosis of Lumbar Spondylosis:
When a patiënt is suffering from low back pain, there are a lot of possible pathologies that could be the cause of this pain. Along with lumbar spondylosis(and its sub-divisions), there are other causes as well, for example:
• Rheumatoid arthritis
We can understand why some clinicians would include rheumatoid arthritis, because there are sub divisions of lumbar spondylosis that have a lot of similarities with arthritis.
• Minor back trauma
As said in the article of Middleton et al., minor back trauma can be the cause of degenerative pathology’s such as spondylosis. It is the job of the physiotherapist to take lumbar spondylosis, and other degenerative diseases for that matter, when a patiënt is diagnosed with a minor back trauma
• Excessive exercise
• Back strain
• Bekhterev’s disease (Ankylosing Spondylitis)
• Coccyx Pain
• Spinal Masses (If the physiotherapist performs a bad investigation, this could be an option, but normally this would be noticed with palpation.)
• Infection
• Disk Herniation
• Discitis
• Lumbar Compression Fracture
• Lumbar Degenerative Disk Disease
• Lumbar Facet Arthropathy
• Mechanical Low Back Pain
• Overuse Injury
Diagnostic Procedures:

LUMBAR SPONDYLOSIS DIAGNOSIS
For the clinical diagnosis of lumbar spondylosis, a thorough investigation is necessary to ensure that other pathologies are excluded. In clinical practice we use:
MRI: expensive, but shows the greatest details in the spine and is used to visualize the intervertebral discs, including the degree of disc herniation, if present. An MRI is also used to visualize the vertebrae, the facet joints, the nerves, and the ligaments in the spine and can reliably diagnose a pinched nerve

MRI OF LS
X-rays: show bone spurs on vertebral bodies in the spine, thickening of facet joints (the joints that connect the vertebrae to each other), and narrowing of the intervertebral disc spaces.

X-RAY OF LS
CT scan: able to visualize the spine in greater detail and can diagnose narrowing of the spinal canal (spinal stenosis) when present
SPECT: Single-photon emission computed tomography bone scintigraphy is used to further evaluate patients with suspected spondylolysis. Controversy surrounds the designation of one of these tests as most useful in the evaluation of spondylolysis.
These procedures were validated in several studies, which concluded that MRI was effective (92% sensitivity) in identifying pars lesions. CT scan was also used as a diagnostic procedure, but the result weren’t equally positive. That’s the reason why MRI is advised as the best method of diagnosis.
Examination:
When a physical therapist performs an examination for lumbar spondylosis, it is advised to follow the principles of the general spine examination and apply them to this specific pathology.
General examination of the spine
• The examination should begin as soon as you first see the patient and continues with careful observation during the whole consultation.
• It is essential to observe the patient’s gait and posture.
Inspection
• Inspection of the entire spine.
• Look for any obvious swellings or surgical scars.
• Assess for deformity: scoliosis, kyphosis, loss of lumbar lordosis or hyperlordosis of the lumbar spine. Look for shoulder asymmetry and pelvic tilt.
Palpation
• Palpate for tenderness over bone and soft tissues.
• Perform an abdominal examination to identify any masses and consider a rectal examination to exclude other pathologies in this region
No tenderness to palpation is noted, but some discomfort can be elicited with deep percussion over the midline of the lumbar area.
Physical findings that may also be present include antalgic or normal gait, tight lumbar musculature and hamstrings, hyperlordosis, and buttock or thigh pain.
Movement
• The normal ranges of movement are outlined in the relevant sections below.
• Examination of the spine must also include examination of the shoulders and examination of the hips to exclude these joints as a cause of the symptoms.
Range of motion is full.
Neurovascular examination
• A thorough examination of sensation, tone, power and reflexes should be performed
• Always consider the possibility of acute spinal cord compression, which is a neurosurgical emergency.
• All peripheral pulses should also be checked, as vascular claudication in the upper and lower limbs can mimic symptoms of radiculopathy or canal stenosis
Forward flexion does not increase symptoms, Sciatica can occur but is rare.
Medical Management :
NSAIDS (=non-steroidal anti-inflammatory drugs) are analgesics and anti-inflammatory. It covers wide range selectivity. From the nonselective cyclooxygenase (COX) inhibitors to the preferential COX-2. It is generally accepted to be the first step in management of lumbar spondylosis.
Opioid medication is an alternative therapy for patients suffering from gastrointestinal side-effects due to a poor control of NSAIDS management. Patients who use this type of medication report greater distress/ suffering and higher functional disability scores.
Antidepressants: have been used for treatment of LBP because of their analgesic value at low doses. The use of antidepressants has also been explored for their dual role in treatment of depression that accompanies lumbar spondylosis syndrome.
Muscle relaxants may provide benefit with regard to short-term pain relief and overall functioning.
- -Taping: Another non chirurgical management could be taping. A lot of studies have already showed that taping helps relieving pain in the lower back. This tape could be standard tape or Kinesio Tape as it is shown that there is no difference between both tapes. It is also important to note that taping alone is not enough, it should be used during the therapy to improve ROM etc.
- Epidural steroid injections are the most common injections and target the epidural space (space surrounding the membrane that covers the spine and nerve roots). These are strong anti-inflammatory (combination of a corticosteroid with a local anesthetic pain relief medicine) and give an immediate pain relief. However, there is poor evidence for the effectiveness (improvement in short-term and long-term benefits) and safety of epidural steroid injections for spinal stenosis.
- Lumbar Facet joint injections are minimally invasive injections of medication (intra-articular injection of local anesthetics with or without steroid) into the inflamed facet joints. This medication can temporarily relieve back pain. It can be used as a diagnostic test or as a treatment to relieve inflammation and pain.
- SI joint injections are used for treatment of sacroiliac joint pain. It consists of injections of local anesthetics and steroids, radiofrequency ablation of the joint capsule, or radiofrequency neurotomy of the lumbosacral lateral branch nerves L5 and S1–S3. No serious complications have been reported after SI joint injection.
Physiotherapy Management in Lumbar Spondylosis:
Goals
- Relief of pain .
- Restoration of movements.
- Strengthening of muscles.
- Education of posture.
- Analysis of precipitating factors to reduce recurrence of the patient’s problems.
Management of acute symptoms:
Rest and Support- With acute joint symptoms, a lumbar corset may be helpful to provide rest to inflamed facet joints. When acute symptoms decrease, discontinue corset by gradually increasing the time without the corset. Often the most comfortable position is flexion, esp. if there are neurologic signs due to decrease in the foraminal space from joint swelling or osteophytes.
- Education of posture- Head, neck and shoulders should be supported by the back rest of chair with a small pillow in the lumbar spine, the feet supported and the arm resting on arm rests or on a pillow in the lap.
- Modalities- Hot or cold packs on the affected area, ultrasound and TENs are some of the other treatments which are used to decrease pain and reduce muscle spasm.
- Relaxation- by soft tissue techniques. Teach self relaxation techniques,e.g like deep breathing exercises and physiological relaxation (Laura Mitchell method) and hydrotherapy.
- Traction- Gentle intermittent joint distraction and gliding techniques may inhibit painful muscle responses and provide synovial fluid movement within the joint for healing.
- Gentle ROM within the limits of pain.
Management of sub-acute and chronic phase:
- Increase ROM- Free active exercises of lumbar spine. Pelvic tilting forward, backward in crook lying, quadriped, sitting and standing.
Mobilization- Restoration of intersegmental mobility by accessory pressure enables the patient to regain full functional pain free movement.
stretching exercises.
Strengthening exercises.
Posture correction. - Manipulation:
Into conservative treatment commonly involves manual therapy, more specifically spine manipulation. Even though the precise mechanism for improvement in low back pain remains unclear, spine manipulation proves to be useful.
On the other hand there might be a risk using spine manipulation, there is a risk of calcifications in the spine should be taken in consideration. Depending the patient condition the risk may be high or low. - TENs:
TENS is a frequently used therapeutic modality. It appears to give an immediate reduction in pain symptoms following the therapy. - Lumbar back supports can be benefit for patients suffering of chronic LBP. It occurs to limit spine motion, stabilize, correct deformity and reduce mechanical forces. There is no consensus if it may function as a placebo or really improve pain and functional ability.
Sitting decreases lumbar lordosis and increase disc pressure, squeeze on the ischium and muscle activity in the lower back. These are all associated with low back pain.Resulted in a diminished lumbar spine load and lumbar muscular activity with lumbar back support. This may possibly lessen low back pain while sitting. It is well-known that chronic spinal pain is often associated with bio-psychosocial problems. Therefore, multidisciplinary back therapy is needed. A bio-psycho-social approach involved reinforcement, modified expectations, imagery/relaxation techniques, and learned control of physiological responses aim to reduce a patient’s perception of disability and pain symptoms.
Also, performing exercises following the McKenzie method could be really helpful. The McKenzie method focuses on extension, and has promising results concerning the prevention of further degeneration of the (lumbar) spine.
It has also been showed in several studies that Yoga could be helpful in reducing pain in patients with chronic low back pain. The stretching of muscles is an important part of this technique. The stretching and relaxing of muscles helps the patients to cope with the pain and relieving them. It should also be noted that Yoga alone is not a therapy for chronic low back pain, it can be an additional technique in the therapy.
Lumbar support of brace:
Lumbar support with the help of braces are used for stabilization and reducing mechanical forces, they are also produced to limit spine motion and correct deformity of the spine. There is limited evidence based research available about the efficacy of lumbar supports regarding to patient improvement and functional ability to go back to work. An example of a brace for Lumbal support is the The Lyon Antikyphosis Brace. This brace has the best results for patients suffering of a scoliosis but could also help patients suffering from lumbar spondylosis. Braces may have effects by massaging and heating the painful areas, there is also a probability that the lumbar supports work as a placebo.

Other Back Exercises:

LOW BACK EXERCISE- BRIDGING
Back exercises are almost always necessary to rehabilitate the spine and alleviate back pain. A controlled, gradual exercise program that is tailored to an individual is usually the most effective.
The abdominal muscles and back muscles are key components of this muscular network, and provide the strength to keep the body upright and for movement. When these core muscles are in poor condition, additional stress is applied to the spine as it supports the body, and back injury or back pain is more likely.
Goals of Back and Abdominal Exercise

BACK FLEXION EXERCISE
Different abdominal and back exercises focus on the muscles that support the spine, which are grouped in three categories:
- Extensors (back and gluteal muscles). These muscles are used to straighten the back (stand), lift and extend, and abduct the hip (move the thigh away from the body).
- Flexors (abdominal and iliopsoas muscles). These muscles are used to bend and support the spine from the front. The flexors also control the arch of the lumbar (lower) spine, and flex and adduct the hip (move the thigh in toward the body).
- Obliques or Rotators (paraspinal (side) muscles). These muscles are used to stabilize the spine when upright. The obliques also rotate the spine and help maintain proper posture and spinal curvature.
To be most effective, abdominal exercises should include focus on working the following muscles:
- The abdominal muscles
- The lower abdominal muscles
- The outside (oblique) muscles
Pelvic Tilt – Lie on floor with knees bent, feet parallel and arms to the side
- Tighten lower abdominal muscles, pulling the navel and lower back toward the floor, without using buttocks or leg muscles
- Hold for 5 seconds
- 5-10 repetitions
Trunk Curl – Lie on floor with knees bent and arms crossed on the chest
- Using upper abdominal muscles, raise trunk of body off the floor slightly, to about 15 degrees
- Hold 5 seconds
- Lower trunk slowly to the floor.
To be effective, motion should raise the chest, rather than the head or neck, and only be only a slight lift. Rising too far, to a sitting position, works leg muscles not the abdominals.
Stretches for Low Back Pain
- Back Flexion Stretch. Lying on the back, pull both knees to the chest while simultaneously flexing the head forward until a comfortable stretch is felt across the mid and low back.
- Knee to Chest Stretch. Lie on the back with the knees bent and both heels on the floor, then place both hands behind one knee and pull it toward the chest, stretching the gluteus and piriformis muscles in the buttock.
- Kneeling Lunge Stretch. Starting on both knees, move one leg forward so the foot is flat on the ground, keeping weight evenly distributed through both hips (rather than on one side or the other). Place both hands on the top of the thigh, and gently lean the body forward to feel a stretch in the front of the other leg. This stretch affects the hip flexor muscles, which attach to the pelvis and can impact posture if too tight.
- Piriformis Muscle Stretch. Lie on the back with knees bent and both heels on the floor. Cross one leg over the other, resting the ankle on the bent knee, then gently pull the bottom knee toward the chest until a stretch is felt in the buttock. Or, lying on the floor, cross one leg over the other and pull it forward over the body at the knee, keeping the other leg flat.
- Hamstring muscle stretch. Tight hamstring muscles are a common contributor to lower back pain. The hamstring muscle run through the back of each thigh from the hip down to the back of the knee.



0Comments