Colposcopy was first described by Hans Hinselman of Germany in 1925 as a screening tool for cervical cancer. Hinselman suspected that endophytic or exophytic lesions of the cervix were likely precursors of cervical carcinoma, and he hoped that by magnifying these tissues, precursor lesions might be identified early enough to allow effective treatment before invasive disease developed or spread. His theories on the genesis of cervical cancer were incorrect, and his protocol for colposcopic evaluation was clinically impractical, so the search for alternative methods for cervical cancer screening continued.
 |
| Colposcopy |
In 1920, Dr. George Papanicolaou began his investigation of vaginal and cervical cytology. In collaboration with Herbert Traut, he published his seminal monograph Diagnosis of Uterine Cancer by the Vaginal Smear in 1943. In the United States, the Papanicolaou test became the primary screening test for detection of cervical cancer and its precursors. Colposcopy was essentially unknown in this country until the 1960s, when it was introduced in its current role as a confirmatory test for evaluation of women with abnormal cervical cytologic findings. Currently, it has near-universal acceptance as the most effective follow-up test for women suspected of having premalignant or malignant cervical lesions.
Until the early 1970s, the usual management of women found to have an abnormal Papanicolaou test result was cone biopsy of the cervix. In most cases, examination of the biopsy specimen revealed only minor epithelial changes. Therefore, most women were being overtreated at significant human, as well as financial, cost. The acceptance of colposcopic evaluation as an intermediate step to identify patients who truly require surgical therapy has resulted in a dramatic decrease in such unnecessary surgery.
The importance of accurate screening and evaluation for cervical cancer cannot be overstated. At the beginning of the 20th century, cervical cancer was the most common cancer to affect women worldwide, as well as the most common malignancy among females in the United States. In large part due to the widespread implementation of effective cervical cytologic screening programs (using the Papanicolaou test), the frequency of cervical cancer has decreased dramatically in the United States. Cervical cancer remains a problem in unscreened populations.
The National Cancer Institute estimates that in 2009 there were 11,270 new cases of cervical cancer diagnosed in the United States, and that approximately 4070 women died of this disease. Additionally, 45,000 women are found to have high-grade premalignant cervical epithelial lesions. Outside the United States, especially in developing countries, the prevalence of cervical cancer remains high. At the end of the 20th century, it remained the secondmost common cause of cancer death in women worldwide.
 |
| Colposcopy |
Etiology
The initiating event for cervical cancer in almost all cases is infection of the cervical epithelium by one of several serotypes of human papillomavirus (HPV). HPV DNA is found in more than 99.7% of all cervical cancers. More than 100 serotypes exist in this family of DNA viruses, approximately 30 of which have a predilection for the female genital tract. Approximately 15 of these serotypes have been found in cervical cancer. Serotypes 16 and 18 account for almost 70% of cervical cancer.
Immunosuppressed women, such as patients with AIDS, and women exposed to certain environmental factors (notably cigarette smoke), are at increased risk.
Pathophysiology
Squamous cell carcinoma accounts for approximately 80% of cervical cancer cases. Significant advances have occurred in the understanding of the pathophysiology and molecular basis of this disease. These advances have resulted in modification of management recommendations. The previously held concept that cervical cancer was the end-stage of an inexorable progression of cervical morphology from atypia through progressively more severe intraepithelial neoplasia to eventually become invasive squamous carcinoma, is overly simplistic.
As noted, the critical step in the initiation of the malignant process is epithelial infection with an oncogenic virus. When a cervical epithelial cell of a susceptible host is infected by one of these high-risk viruses, the viral genome is incorporated into the host cell genome. Inactivation of the p53 tumor suppressor gene and retinoblastoma gene by the viral genome results in immortalization of the infected cells. Absent effective immune surveillance by the host, the affected tissue may eventually undergo malignant transformation. These patients typically present with higher-grade lesions (CIN II, III, or frank cancer).
Conversely, low-grade cervical intraepithelial neoplasia (CIN I) lesions are almost always the result of infection with a nononcogenic virus, typically serotypes 6 and 11. Infection of cervical epithelial cells by one of these serotypes may result in exuberant cell proliferation during the course of viral replication (essentially resulting in formation of a wart), and these patients will present with CIN I lesions. However, the normal process of cell maturation and apoptosis is preserved, and malignant transformation is very rare. Spontaneous resolution of CIN I lesions is common. Conversely, spontaneous resolution of higher-grade lesions becomes progressively less certain, and active therapy is usually indicated.
 |
| Colposcopy |
Indications
Colposcopic evaluation is indicated when the presence of a malignant or premalignant lesion in the cervix, vagina, or vulva is suspected. Uncommonly, this situation may arise when an unusual cervical lesion is detected as the result of inspection of the vagina and cervix for an unrelated reason.
Another specific indication is evaluation of a patient who presents with postcoital vaginal bleeding. Although this symptom is most commonly the result of vaginal or cervical trauma, postcoital bleeding is a classic symptom of cervical cancer.
The most common situation arises as the result of cervical cytological screening as part of a routine health maintenance evaluation.
Almost all United States cytopathology laboratories use the Bethesda System for reporting findings of cervical cytology. The version in current use is the 2001 revision.
Following are pertinent components of reports issued under this system:
Specimen adequacy
Presence or absence of endocervical or transformation
Zone components
General categorization
Negative for intraepithelial lesion or malignancyEpithelial cell abnormality
Interpretation/result
Epithelial cell abnormality
Atypical squamous cells, undeterminedsignificance (ASC-US)
Atypical squamous cells, cannot exclude high-grade squamous intraepithelial lesion (ASC-H)
Low-grade squamous intraepithelial lesion (LSIL)
High-grade squamous intraepithelial lesion (HSIL)
Squamous cell carcinoma
Glandular cell abnormality
Atypical glandular cells (AGC)Endocervical adenocarcinoma in situ (AIS)
Adenocarcinoma
Evaluation of the patient with an abnormal pap smear has been evolving. In September 2006, a panel of experts representing 29 organizations and professional societies issued a set of consensus guidelines reflecting current understanding of the pathophysiology and natural history of cervical dysplasia
Importantly, the cytologic classifications do not correspond to histologic evaluation of tissue samples, and patient management ultimately must be based on histologic diagnosis. In the special case of adolescent women, who are at very low risk for epithelial cervical cancer, and in whom low-grade changes usually resolve spontaneously, colposcopy is recommended to be reserved for high-grade SIL. In the special case of pregnant women, deferring colposcopy until after delivery is reasonable unless cytologic evaluation suggests significant risk of invasive disease.
 |
| Colposcopy |
They may be summarized as follows:
Negative for intraepithelial abnormality: These patients should continue to receive routine cytologic screening.ASC-H, LGSIL, HGSIL, squamous cell cancer: Because of the increased incidence of significant histologic abnormality in patients who have these diagnoses, colposcopic evaluation and biopsy of abnormal sites is recommended. In the special case of postmenopausal women, atrophic changes may result in the cytologic diagnosis of LGSIL. Managing these women similar to those with a diagnosis of ASC-US is appropriate.
ASC-US: As with the other abnormal Papanicolaou test classification, colposcopic evaluation is an option. However, because this is the least reproducible of the cytologic categories, and because of the very low risk of invasive cancer in patients who have this diagnosis, less aggressive management strategies are also options. These include the following:
Repeat cytologic evaluation at 6 and 12 months“Reflex” testing for the presence of high-risk HPV serotypes.
If either of these strategies results in abnormal findings, colposcopy is indicated. Should no abnormality be discerned, the patient may resume routine surveillance.
AGC: This finding is not uncommonly associated with significant glandular or squamous cell abnormality somewhere in the lower genital tract. As neither repeat cytologic testing nor HPV testing has been found to have sufficient sensitivity to detect endocervical or endometrial abnormalities, these patients are recommended to undergo colposcopic, endocervical and endometrial evaluation, and sampling in addition to HPV testing.
AIS, adenocarcinoma: These patients may require excisional procedures to assure adequate sampling should the above measures not be diagnostic.
Relevant Anatomy
The ring of cervical epithelium between the native squamous epithelium of the outer cervix (or cervical portio) and the columnar epithelium of the endocervical canal is a region of significant morphologic fluctuation.
The columnar epithelium of the endocervical canal often extends out onto the cervical portio prior to menarche. Under the influence of environmental factors in the vagina, especially increased acidity associated with menarche, the exposed columnar epithelium undergoes morphologic change referred to as squamous metaplasia, a thin layer of stratified squamous epithelium overlying the columnar epithelium. See the image below
 |
| Early metaplastic change of columnar epithelium. |
The ring of squamous metaplasia is referred to as the transformation zone. The border between the metaplastic epithelium and the endocervical columnar epithelium is referred to as the squamocolumnar junction. Because viral infections most commonly affect cells in rapidly dividing epithelium, the transformation zone is typically the locus of dysplastic change. Therefore, complete visualization of the entire transformation zone, most specifically the squamocolumnar junction is required for adequate assessment.
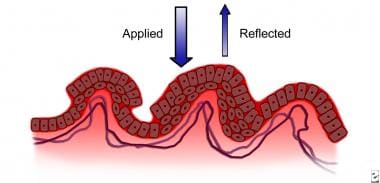
Colposcopic evaluation is aided by the differential reaction of the cells of mature squamous tissue and actively dividing squamous tissue to dilute acetic acid and iodine. Actively dividing cells are characterized by an increased nuclear–cytoplasm ratio. This is especially true of HPV–infected cells (see image below).
 |
| Human papilloma virus (HPV)–infected epithelium with increased light reflectance. |
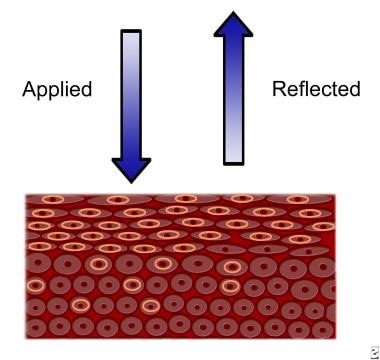
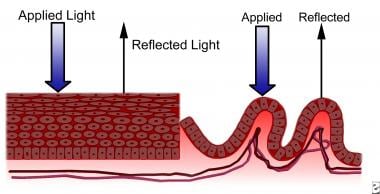
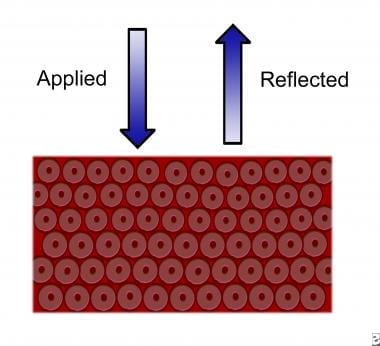
Exposure of such tissue to dilute acetic acid results in increased light reflectivity and, therefore, visual contrast with normal tissue (see image below). Mature squamous epithelial cells contain a large amount of glycogen, which stains a characteristic mahogany color when exposed to iodine (the Schiller reaction), whereas rapidly dividing cells, which contain relatively little glycogen, remain unstained.
 |
| Normal squamocolumnar junction. Tissue response to applied light. |
Another hallmark of intraepithelial neoplasia and invasive disease is alteration of the microvasculature of the transformation zone. Columnar epithelium is characterized by a single layer of columnar cells overlying stromal fronds. Each of these villous fronds protruding into the columnar-lined endocervix has its own capillary supply.
During the process of squamous metaplasia, these vessels become covered over and therefore less visible. Cellular proliferation associated with viral infection or dysplastic transformation (shown in the image below) is associated with vascular changes.
 |
| Dysplastic epithelium with increased reflectance of applied light. |
There is in-growth of the perpendicular vessels into the epithelium. Viewed end-on under magnification, these vessels appear as small red dots (referred to as “punctation,” depicted in the image below).
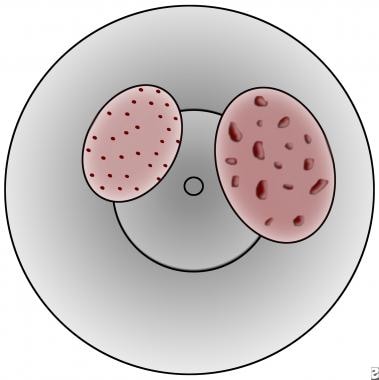 |
| Punctation in cervical lesions. Left is fine, right is coarse (likely high grade or invasive). |
The vessels can become interconnected in intricate patterns that resemble a tiled floor (referred to as “mosaicism”, depicted in the image below).
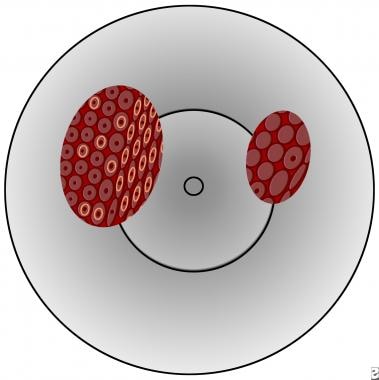 |
| Mosaicism in cervical lesions; left is fine, right is coarse (likely high grade or invasive). |
Some relationship appears to exist between increased vascular spacing and degree of dysplasia, but this has proven to be an insensitive marker. On the other hand, the presence of a vessel course irregularity (eg, sudden vessel termination, “hairpin” or “comma” type vessels, abnormal branching, or increasing diameter of a vessel previously diminishing in caliber) is suggestive of malignant transformation.
Contraindications
No absolute contraindications to the performance of a colposcopic examination exist, although special precautions may be required in special circumstances, such as a pregnant patient who harbors a placenta previa. The patient's ability to tolerate a standard speculum examination is the only true limiting factor. Pregnancy by itself is not a contraindication. Active cervicitis and vulvovaginitis should be treated before undertaking the examination, because inflamed tissues can alter the ability to obtain an accurate assessment, and it can also make the discomfort of the examination markedly worse.



0Comments