The use of echocardiography as an imaging modality has increased substantially over the past decade. Cardiologists perform most echocardiography studies, with internists being the next most common providers of these studies (15% of all Medicare charges submitted for the procedure). The objective of this article is to provide clinicians with a brief review of basic principles and instrumentation of echocardiography.
 |
| Echocardiography |
Neither bone nor air is a good transmission medium for ultrasound waves; accordingly, specific windows (eg, apical, parasternal, subcostal, and suprasternal) are used to image the heart.
Two-dimensional (2-D) and 3-D echocardiography provide real-time imaging of heart structures throughout the cardiac cycle. Doppler echocardiography provides information on blood movement inside cardiac structures and on hemodynamics.
Tissue Doppler imaging (TDI) provides information about movement of cardiac structures. The relation between the dynamics of cardiac structures and the hemodynamics of the blood inside these structures provides information about cardiac diastolic and systolic function. Echocardiography is continuously evolving and constantly being augmented by newer modalities, such as tissue harmonics, speckle tracking, tissue Doppler strain, and tissue characterization.
The advent of myocardial perfusion echocardiography (MCE) has allowed functional evaluation of the coronary microcirculation, including quantitative coronary blood flow and fractional flow reserve. [2] This has helped to improve "the definition of ischemic burden and the relative contribution of collaterals in noncritical coronary stenosis." Moreover, MCE identifies no-reflow within myocardial infarctions (MIs) and low-flow around MIs, predicts potential functional recovery of stunned myocardium with appropriate interventions, and appears to have a diagnostic performance comparable to positron emission tomography (PET) scanning in microvascular reserve/dysfunction in angina patients.
Dedicated training for competent performance and interpretation of echocardiography is essential. The American College of Cardiology (ACC) and the American Heart Association (AHA) have recommended a set of minimum knowledge and training requirements for the performance and interpretation of echocardiography, including a minimum number of 150 performed and 300 interpreted examinations for basic level II (for level III: 300 performed/750 interpreted) in interpreting echocardiography. Similar guidelines have been developed in Canada.
Basic principles of echocardiography
Humans can hear sound waves with frequencies ranging from 20 to 20,000 cycles per second—that is, from 20 Hertz (Hz) to 20 kHz. Frequencies higher than 20 kHz are referred to as ultrasound. Diagnostic medical ultrasonography usually uses transducers with frequencies of 1-20 MHz. Ultrasound waves are described in terms of the following features:
Frequency (Hz)Wavelength (mm)
Amplitude, or loudness (decibels [dB])
These phenomena are the basis for many of the clinical applications and calculations of echocardiography.
Interaction of ultrasound waves with tissue results in reflection, scattering, refraction, and attenuation of the waves. 2-D echocardiographic imaging is based on reflection of transmitted ultrasound waves. Doppler analysis is based on the scattering of ultrasound waves from moving blood cells, with a resulting change in the frequency of the waves received at the transducer. Attenuation limits the depth of ultrasound penetration. Refraction, a change in the direction of the ultrasound wave, results in imaging artifacts.
Because wavelength (λ) times frequency (ƒ) equals the propagation velocity (с), or λ × ƒ = с, and the propagation velocity in the heart is 1540 m/sec, the wavelength for any transducer frequency can be calculated as follows:
λ (mm) = 1.54/ƒ (MHz)
Wavelength has clinical importance, in that image resolution cannot be greater than 1-2 wavelengths. That is to say, the higher the frequency, the shorter the wavelength and the better the image resolution.
The depth to which ultrasound waves penetrate the body is directly related to wavelength (ie, shorter wavelengths penetrate a shorter distance). [8] The depth of penetration for adequate imaging tends to be limited to about 200 wavelengths. Thus, an obvious tradeoff exists between image resolution and depth of penetration. Thus, a 1-MHz transducer has a penetration depth of 30 cm and resolution of 1.5 mm, whereas a 5-MHz transducer has a lesser penetration depth, only 6 cm, but a higher resolution, approximately 0.3 mm.
2-D imaging depends on reflection of ultrasound waves. These waves are reflected at tissue boundaries and interfaces, with the quantity dependent on the relative change in acoustic impedance (ie, density) between the two tissues. Optimal return of reflected ultrasound waves occurs at a perpendicular angle (90°).
Doppler flow imaging depends on the scattering phenomenon, and its optimal flow angle is the opposite of that for 2-D imaging (ie, parallel to the flow of interest, rather than perpendicular). The Doppler effect may be simply stated as follows: A person moving toward a sound source will hear a tone with higher frequency than the emitted wave frequency, whereas a person moving away from the source of sound will hear the tone with a lower frequency than the emitted wave frequency.
Additional common terms and concepts employed in echocardiography include the following:
Duty factor - The fraction of time during which a transducer is sending an ultrasound impulseIndications
The ACC, the AHA, and the American Society of Echocardiography (ASE) have published detailed practice guidelines for the clinical application of echocardiography. [9] More recently, these and other bodies have collaborated to establish appropriate use criteria for echocardiography. [10]
Briefly, indications of echocardiography may be divided into structural imaging and hemodynamic imaging. Indications for structural imaging include the following:
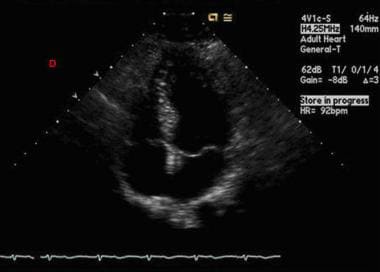
Structural imaging of the pericardium (eg, to exclude pericardial effusion)Structural imaging of atria and septa between cardiac chambers (eg, congenital heart disease, traumatic heart disease; see the second image below)
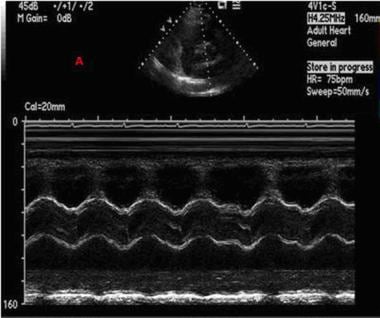 |
| Echocardiography. This is an M-mode image across the aortic valve as well as the left atrium plotted against time. |
Indications for hemodynamic imaging through Doppler techniques include the following:
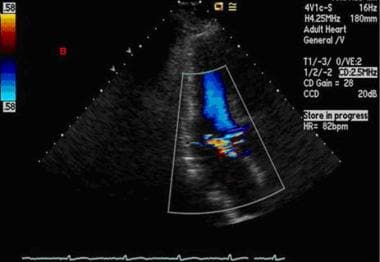
Imaging of blood flow through heart valves (eg, valvular stenosis and regurgitation; see the image below)Imaging of blood flow through the cardiac chambers (eg, cardiac output calculation, assessment of diastolic and systolic function of the heart)
Tissue Doppler imaging of heart structures - This, compared with Doppler imaging of blood flow through these structures, provides valuable information about the dynamics of heart function; for example, in diastolic dysfunction, an increased ratio of early transmitral Doppler blood flow to early mitral annulus tissue Doppler indicates that a high intra-atrial pressure is an important driving force
Contraindications
Echocardiography has no contraindications. It should be kept in mind, however, that this modality may yield only limited information in patients at the extremes of adult body weight, because a thick chest wall (in markedly obese patients) or overcrowded ribs (in severely underweight patients) may limit the penetration of ultrasound waves.
Technical Considerations
The following considerations should be kept in mind in the performance of echocardiography:
Transducer selection - Although each transducer has a stated frequency, with each burst it actually emits a range of different ultrasound wave frequencies, and this range is called its frequency bandwidth; a wider emitted bandwidth yields better resolution of distant structures and also allows a short pulse, thus avoiding overlap between the reflected ultrasound signals; a smaller transducer "footprint" or aperture size is an advantage, in that it facilitates use in narrow intercostal spacesDepth adjustment - To improve resolution, depth should be decreased to the minimum needed to visualize the structure of interest; in an average adult, a depth of 16 cm is usually adequate for the apical view, and a depth of 12 cm suffices for the parasternal view
Transducer frequency - This should adjusted to the maximum that permits adequate depth penetration
Time gain compensation (TGC) - This function should be set in the midrange, with lower gain in the near field and higher setting in the far field to compensate for attenuation of the beam at higher depths
Tissue harmonics - Harmonic imaging can result in a false appearance of a thickened valve leaflet; if there is doubt about the actual valve thickness, the tissue harmonics feature should be turned off and a reassessment made
Transmit gain/output - This should be adjusted to optimize image brightness; if emitted energy is too low, everything appears black, but if it is too high, a whiteout results; it should initially be set to high and then adjusted downward
Dynamic range/compress function - If image is quality is poor, this function should be decreased to produce better contrast images; on the other hand, increasing the setting of this function softens the images
Focus function - This is used to clarify a structure of specific interest (eg, an apical thrombus in the left ventricle); when the beam is focused, it is adjusted to be narrowest at the area of interest, resulting in better resolution
Electrocardiography (ECG) lead placement - Because digital echocardiography stores few cycles for each view, ectopic beats can result in a false impression about wall motion or ventricular function; for example, a postectopic beat compensatory period may falsely increase the ejection fraction or Doppler transvalvular gradient; in general, store beats without ectopic activity, and in atrial fibrillation, record at least 7-10 beats
Contrast agents - These should be considered for improving endocardial delineation
Timing - Images should be obtained at end-expiration, when the heart is closer to the transducer
A good continuous Doppler signal should yield a Doppler spectral signal that has a smooth contour with well-defined edge, onset, and end of flow; the display is "filled in" because lower-velocity signals throughout the pathway of the beam are captured by the continuous beam; the audible signal is tonal and smooth




0Comments