Coronary artery disease is a narrowing or blockage of your coronary arteries usually caused by the buildup of fatty material called plaque. Coronary artery disease is also called coronary heart disease, ischemic heart disease and heart disease.
 |
| Coronary Artery Disease |
Where are the coronary arteries? What do they do?
Coronary arteries are the blood vessels that supply oxygen-rich blood to your heart muscle to keep it pumping. The coronary arteries are directly on top of your heart muscle. You have four main coronary arteries:
- The right coronary artery.
- The left coronary artery.
- The left anterior descending artery.
- The left circumflex artery.
What happens to the arteries in coronary artery disease?
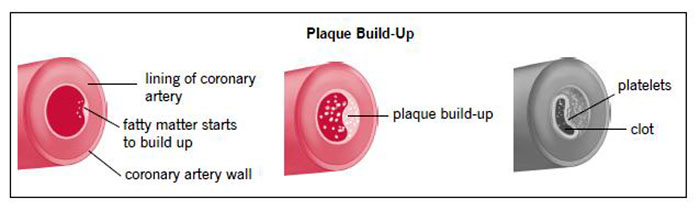
Coronary artery disease is caused by atherosclerosis. Atherosclerosis is the buildup of plaque inside your arteries. Plaque consists of cholesterol, fatty substances, waste products, calcium and the clot-making substance fibrin. As plaque continues to collect on your artery walls, your arteries narrow and stiffen. Plaque can clog or damage your arteries, which limits or stops blood flow to your heart muscle. If your heart does not get enough blood, it can't get the oxygen and nutrients it needs to work properly. This condition is called ischemia. Not getting enough blood supply to your heart muscle can lead to chest discomfort or chest pain (called angina). It also puts you at risk for a heart attack.
How does plaque build up in the arteries?
Coronary artery disease happens in everyone. The speed at which it develops differs from person to person. The process usually starts when you are very young. Before your teen years, the blood vessel walls start to show streaks of fat. As plaque deposits in your artery’s inner walls, your body fights back against this ongoing process by sending white blood cells to attack the cholesterol, but the attack causes more inflammation. This triggers yet other cells in the artery wall to form a soft cap over the plaque.
This thin cap over the plaque can break open (due to blood pressure or other causes). Blood cell fragments called platelets stick to the site of “the injury,” causing a clot to form. The clot further narrows arteries. Sometimes a blood clot breaks apart on its own. Other times the clot blocks blood flow through the artery, depriving the heart of oxygen and causing a heart attack.
The process of how plaque builds up in your coronary arteries.
Who gets coronary artery disease?
You have an increased risk of coronary artery disease if you:
- Have a high cholesterol level (especially a high LDL “bad” cholesterol level and a low HDL “good” cholesterol level).
- Have high blood pressure.
- Family history of heart disease.
- Have diabetes.
- Are a smoker.
- Are a man over 45 years of age or a post-menopausal woman.
- Are overweight.
- Are physically inactive.
- Are an African American, Mexican American, Native American, Native Hawaiian or an Asian American. The increased risks are caused by higher rates of high blood pressure, obesity and diabetes in these populations.
If you have these risk factors, talk with your healthcare provider. They may want to test you for coronary artery disease.
SYMPTOMS AND CAUSES
What are the symptoms of coronary artery disease?
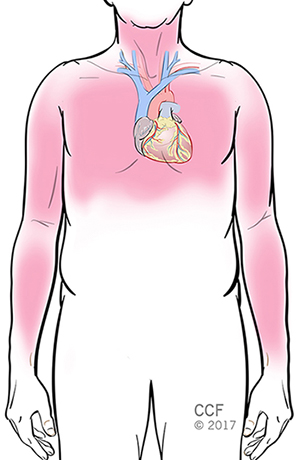
You may not know you have coronary artery disease since you may not have symptoms at first. The buildup of plaque in your arteries takes years to decades. But as your arteries narrow, you may notice mild symptoms that indicate your heart is pumping harder to deliver oxygen-rich blood to your body. The most common symptoms are chest pain or shortness of breath, especially after light physical activity like walking up stairs, but even at rest.
Sometimes you won’t know you have coronary artery disease until you have a heart attack. Symptoms of a heart attack include:
- Chest discomfort (angina) described as heaviness, tightness, pressure, aching, burning, numbness, fullness, squeezing or a dull ache. The discomfort can also spread to or only be felt in your left shoulder, arms, neck, back or jaw.
- Feeling tired.
- Dizziness, lightheadedness.
- Nausea.
- Weakness.
Symptoms of heart attack in women can be slightly different and include:
- Discomfort or pain in the shoulders, neck, abdomen (belly) and/or back.
- Feeling of indigestion or heartburn.
- Unexplained anxiety.
- Cold sweat.
What should I do if I have symptoms of coronary artery disease?
Because the symptoms of coronary artery disease can be symptoms of a heart attack, you need to seek immediate help. CALL 911 if you think you are having symptoms of a heart attack.
If a blood clot in a coronary artery has broken loose and moved into your brain, it can cause a stroke, although this is rare. Symptoms of a stroke include:
- Drooping on one side of your face. Look at your smile in a mirror or ask someone to check your smile.
- Arm weakness or numbness.
- Difficulty speaking/slurred speech.
If you experience any of these symptoms, CALL 911. Every minute you spend without treatment increases your risk of long-term damage.
DIAGNOSIS AND TESTS
How is coronary artery disease diagnosed?
First, unless your condition is an emergency (you’re having a heart attack or stroke), your cardiologist (heart doctor) will ask you about your symptoms, take your medical history, review your risk factors and perform a physical exam.
Diagnostic tests may include:
- Electrocardiograph tests (EKG): This test records the electrical activity of the heart. Can detect heart attack, ischemia and heart rhythm issues.
- Exercise stress tests: This is a treadmill test to determine how well your heart functions when it’s working the hardest. Can detect angina and coronary blockages.
- Pharmacologic stress test: Instead of using exercise to test your heart when it is working its hardest, medication is given to increase your heart rate and mimic exercise. This test can detect angina and coronary blockages.
- Coronary calcium scan: This test measures the amount of calcium in the walls of your coronary arteries, which can be a sign of atherosclerosis.
- Echocardiogram: This test uses sound waves to see how well structures of your heart are working and overall function of your heart.
- Blood tests: Many blood tests are ordered for factors that affect arteries, such as triglycerides, cholesterol, lipoprotein, C-reactive protein, glucose, HbA1c (a measure of diabetic control) and other tests.
- Cardiac catheterization: This test involves inserting small tubes into the blood vessels of the heart to evaluate heart function including the presence of coronary artery disease.
Other diagnostic imaging tests may include:
- Nuclear imaging: This test produces images of the heart after administering a radioactive tracer.
- Computed tomography angiogram: Uses CT and contrast dye to view 3D pictures of the moving heart and detect blockages in the coronary arteries.
MANAGEMENT AND TREATMENT
How is coronary artery disease treated?
Your healthcare provider will talk to you about the best treatment plan for you. Follow your treatment plan to reduce your risk of problems that can result from coronary artery disease, like heart attack and stroke.
Lifestyle changes
The first step in treating coronary artery disease is to reduce your risk factors. This involves making changes in your lifestyle.
- Don’t smoke. If you smoke or use tobacco products, quit. Ask your healthcare providers about ways to quit, including programs and medications.
- Manage health problems like high cholesterol, high blood pressure and diabetes.
- Eat a heart-healthy diet. Talk to your healthcare provider or a registered dietitian about ways to change your diet to reduce your risk of heart disease. Good dietary choices include the Mediterranean and DASH diets.
- Limit alcohol use. Limit daily drinks to no more than one drink per day for women and two drinks per day for men.
- Increase your activity level. Exercise helps you lose weight, improve your physical condition and relieve stress. Most people can reduce their risk of heart attack by doing 30 minutes of walking five times per week or walking 10,000 steps per day. Talk to your healthcare provider before you start any exercise program.
Medications
Your healthcare provider will recommend medications to best manage your risk factors for heart disease. Types of heart-related medications that may be selected for you include:
- Medication to lower your cholesterol level, such as statins, bile acid sequestrants, niacin and fibrates.
- Medications to lower blood pressure, such as beta blockers, calcium channel blockers, angiotensin converting enzyme (ACE) inhibitors or angiotensin II receptor blockers.
- Medications to stop angina, such as nitrates/nitroglycerin or ranolazine.
- Medications to reduce the risk of blood clots, such as anticoagulants (including aspirin) and antiplatelets.
If you have diabetes and coronary artery disease, you’ll be prescribed medications to lower your blood sugar level.
It is important to take all medications as prescribed – those for heart disease and all other health conditions. Talk to your healthcare provider if you have any questions or concerns about which medications to take or how to take them.
Procedures and surgery
Interventional procedures are nonsurgical treatments to get rid of plaque buildup in the arteries and prevent blockages. Common procedures are balloon angioplasty and stenting. These procedures are done with a long, thin tube called a catheter. It is inserted into an artery in the wrist or the top of the leg through a small incision and guided to the blocked or narrowed area of the artery. The balloon widens the diameter of the artery to restore blood flow to the heart. A stent (a small metal spring-like scaffold) is left in place to keep your artery open.
Coronary artery bypass graft (CABG) surgery involves creating a new path for blood to flow when there is a blockage in the coronary arteries. In most cases, the surgeon removes blood vessels from your chest, arm or leg, and creates the new pathway to deliver oxygen-rich blood to the heart.
If traditional treatment options are not successful, your cardiologist may recommend other treatment options, such as enhanced external counterpulsation (EECP). In this procedure, inflatable cuffs (like blood pressure cuffs) are used to squeeze the blood vessels in your lower body. This helps improve blood flow to the heart and helps create natural bypasses (collateral circulation) around blocked coronary arteries. Enhanced external counterpulsation is a possible treatment for those with chronic stable angina who can’t have an invasive procedure or bypass surgery and do not get relief from medication.
Collateral circulation around a blocked coronary artery.
What are the complications of coronary artery disease?
Coronary artery disease can lead to the following other heart conditions:
- Angina.
- Heart attack.
- Heart rhythm problems.
- Heart failure.
- Cardiogenic shock.
- Sudden cardiac arrest.
You can reduce your chance of developing these heart conditions if you follow your cardiologist’s treatment plan.
PREVENTION
Can coronary artery disease be prevented?
You can certainly make changes that will lower your chance of developing coronary artery disease, but this condition is not 100% preventable. This is because there are two kinds of risk factors – those that can’t be changed (nonmodifiable) and those that can be (modifiable).
Nonmodifiable risk factors include older age, male gender, a family history of heart disease and genetic factors. See the question, “who gets coronary artery disease” earlier in this article for more information.
However, there are many risk factors that you can modify. These are mostly lifestyle changes like losing weight if you’re overweight, stopping smoking if you smoke, keeping your blood pressure and cholesterol level at their goal numbers and managing diabetes. See “lifestyle changes” under the treatment section of this article for more examples.
Keep in mind that the more risk factors you have, the higher the chance of having heart disease. Fortunately, you can choose to help yourself and reduce the risk of disease by taking control over your individual risk factors that can be changed.
OUTLOOK / PROGNOSIS
What should I expect if I have coronary artery disease? Can it be cured?
Technically coronary artery disease can’t be cured. If you’ve been diagnosed with coronary artery disease, follow your healthcare provider’s treatment plan to help prevent your condition from getting worse. Your treatment plan may include procedures and surgery to increase the blood supply to your heart, lifestyle changes to target your risk factors and medications.
If your coronary artery disease has led to a heart attack, your healthcare provider can recommend a cardiac rehabilitation program to reduce your risk of future heart problems, regain strength and improve the quality of your life.
It is important to keep all follow-up appointments and have all tests ordered by your healthcare provider. These are needed to keep track of your condition, monitor how well your treatment plan is working and make adjustments if needed.
LIVING WITH
What is acute coronary syndrome?
Acute coronary syndrome is the name given to types of coronary disease that are associated with a sudden blockage in the blood supply to your heart. Some people have symptoms before they have acute coronary syndrome, but you may not have symptoms until the condition occurs. Some people never have any symptoms. Changes caused by acute coronary syndrome can be seen on an electrocardiogram (ECG) and in blood tests. Acute coronary syndrome is defined by the location of the blockage, length of time the artery is blocked and amount of damage and is defined as:
- Unstable angina: This may be a new symptom or can happen if you have stable angina that changes to unstable angina. You may start to have angina more often, when you are resting, or it may be worse or last longer. The condition can lead to a heart attack. If you have unstable angina, you will need medication, such as nitroglycerin or a procedure to correct the problem.
- Non-ST segment elevation myocardial infarction (NSTEMI): This is a type of heart attack (MI) that does not cause major changes on an ECG. But, a blood test will show that there is damage to your heart muscle.
- ST segment elevation myocardial infarction (STEMI): This type of heart attack (MI) is caused by a sudden blockage of the blood supply to the heart.


0Comments