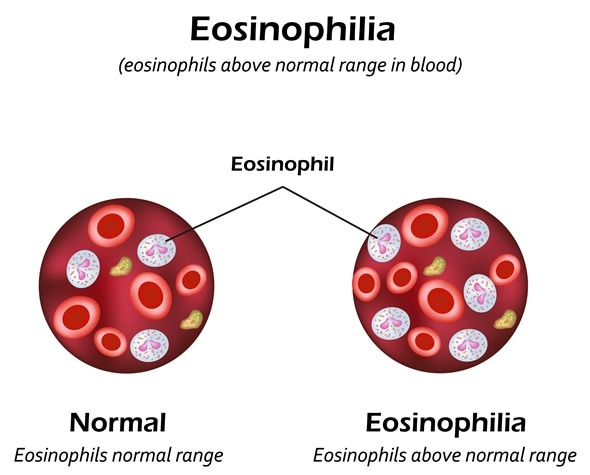
Eosinophils are a type of blood cells which helps to fight off certain infections and participates in the body’s immune reactions.
Eosinophilia is a condition in which the peripheral blood contains an excessive number of eosinophils, more than 500/µL. It may be classified into mild (500-1500/µL); moderate (1500-5000/µL); and severe (over 5000/µL) eosinophilia.
Types of Eosinophilia
Eosinophilia is termed primary or secondary, with respect to its causation. Primary eosinophilia is further classified into clonal eosinophilia, in which there is bone marrow proliferation, and the idiopathic type, which is a diagnosis arrived at when there is no evidence of either clonal or secondary eosinophilia.
Secondary eosinophilia may be due to many reasons. The most common associated conditions include infestations with various parasites, such as microfilaria, and allergic disorders.
There is a set of rare disorders characterized by eosinophilia above 1500/µL persisting for at least 6 months, associated with organ dysfunction, but without other identifiable causes, called the hypereosinophilic syndromes (HES).
Causes of Secondary Eosinophilia
The following list names some diseases which may show eosinophilia in addition to other findings:
- Allergic conditions, especially of the skin and the respiratory tract, such as atopy
- Connective tissue disorders such as Dressler syndrome
- Certain tumors, such as Hodgkin’s disease, also result in eosinophilia.
- Almost all invasive parasite infestations result in a rise in the number of peripheral blood eosinophils, such as ascariasis.
- Non-parasitic infestations such as aspergillosis may also produce a rise in the eosinophil count
- Skin disorders due to hypersensitivity reactions such as pemphigus show associated eosinophilia.
- Syndromes of pulmonary eosinophilic infiltrate with eosinophilia are also rare causes, such as Churg-Strauss syndrome.
- Other conditions such as liver cirrhosis also show eosinophilia.
Symptoms
Eosinophilia may be completely asymptomatic, especially with counts below 1500/µL.However, with markedly high counts, organ damage may occur.
On the other hand, secondary eosinophilia may be associated with symptoms of the underlying conditions.
Mechanisms of Eosinophilia and Tissue Damage
Allergic reactions are associated with a raised eosinophil count, slight at first but increasing with each exposure. Mast cells and basophils associated with a hypersensitivity reaction produce and release a number of cytokines, which evoke IgE production. IgE, in turn, stimulates eosinophil production. IL-5 is a chemokine that is extremely important in the final differentiation of mature eosinophils, as well as their recruitment into sites of inflammation, and their prolonged survival.
In addition, eosinophils produce growth factors which are responsible for the fibrotic response to inflammatory injury in affected tissues. This is because the eosinophils release cytokines which not only induce inflammation, but also attract more eosinophils and other immune cells of various types to the organ site. The release of various chemicals and reactive oxygen species by the eosinophils and other cells creates more tissue damage.
Diagnosis and Treatment
Diagnosis requires a thorough history of travel, drug exposure, allergies and the use of herbal or medicinal supplements. Symptoms such as fever, joint pain or swelling, urinary discoloration, skin rashes or lymph node enlargement need to be elicited. A detailed physical examination will focus on any specific symptoms. Further laboratory testing may include stool testing for parasite ova, as well as organ-specific tests such as a chest X ray or urinalysis.
Treatment is based on cessation of exposure to any identified underlying condition, or to any drug or supplement. In many cases, no primary cause is found, suggesting that eosinophilia is secondary to allergy or parasitosis. In such cases, a brief trial of low-dose corticosteroids often lowers the eosinophil count, confirming the secondary nature of the raised eosinophil count.

0Comments