On June 14, the American Medical Association adopted a new policy, calling on doctors to deemphasise the role of body mass index, or BMI, in clinical practice. The statement by the American Medical Association, the nation’s largest association representing physicians, signals a significant shift in how clinicians regard BMI as a measure of general health. With over 40% of Americans having obesity as defined by BMI, a movement away from BMI could have broad implications for patient care.
BMI basics
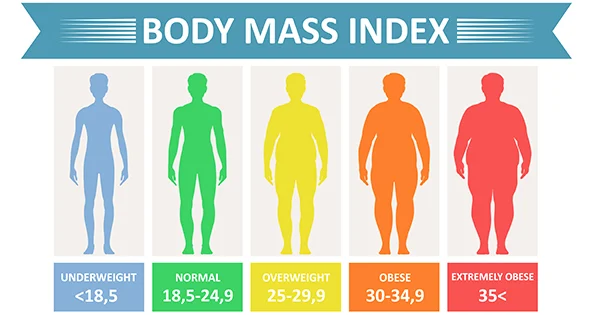
Body mass index is a measurement taken by dividing body weight in kilogrammes by height in metres squared. The metric was developed to estimate a normal body weight depending on an individual’s height, given that taller people tend to weigh more.
It rose to prominence for clinicians in the 1990s following the World Health Organization’s adoption of the metric as the official screening index for obesity.
Research has consistently shown that BMI at a population level correlates strongly with body fat percentage and risk for serious health conditions. The index is easy to measure and inexpensive to calculate, allowing its wide implementation in health care settings.
The House of Delegates adopted new policy recognizing the issues with using BMI as a measurement because:
- Of the historical harm of BMI.
- Of the use of BMI for racist exclusion.
BMI cutoffs are based primarily on data collected from previous generations of non-Hispanic white populations and does not consider a person’s gender or ethnicity.
In addition, the policy says, there are significant limitations associated with the widespread use of BMI in clinical settings and suggests its use be in a conjunction with other valid measures of risk such as, but not limited to, measurements of:
- Visceral fat.
- Body adiposity index.
- Body composition.
- Relative fat mass.
- Waist circumference.
- Genetic or metabolic factors.
The newly adopted AMA policy also states that:
- BMI is significantly correlated with the amount of fat mass in the general population but loses predictability when applied on the individual level.
- Relative body shape and composition heterogeneity across race and ethnic groups, sexes, genders and age-span is essential to consider when applying BMI as a measure of adiposity.
- The use of BMI should not be used as a sole criterion to deny appropriate insurance reimbursement.
This article was first published on The Conversation.



0Comments