Peripheral arterial disease (PAD) -- also known as peripheral vascular disease, atherosclerosis or hardening of the arteries -- is a disorder that occurs in the arteries of the circulatory system. Arteries are the blood vessels that carry oxygen and nutrient-rich blood from the heart to all areas of the body. PAD occurs in the arteries that carry blood to the arms and legs.

Peripheral Arterial Disease (PAD)
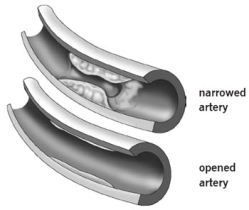
Healthy arteries have a smooth lining that prevents blood from clotting and promotes steady blood flow. In PAD, the arteries slowly become narrowed or blocked when plaque gradually forms inside the artery walls. Plaque is made of excessive fat, cholesterol and other substances floating through the bloodstream, such as inflammatory cells, proteins and calcium. If the arteries become narrowed or blocked, blood cannot get through to nourish organs and other tissues, causing damage to the tissues and eventually tissue death.
The rate at which PAD progresses varies with each individual and depends on many factors, including where in the body the plaque has formed and the person’s overall health.
What are the conditions associated with PAD?
If left untreated, patients with PAD can develop serious health problems, including:
- Heart attack: permanent damage to the heart muscle caused by a lack of blood supply to the heart for an extended time
- Stroke: interruption of the blood flow to the brain
- Transient ischemic attack (TIA): a temporary interruption in the blood supply to the brain)
- Renal artery disease or stenosis: a narrowing or blockage of the artery that supplies blood to the kidney
- Amputation: the removal of part or all of the foot or leg (rarely the arm), especially in people who also have diabetes
Development of Peripheral Arterial Disease
Your arteries are shaped like hollow tubes. Inside, they are smooth and elastic, allowing blood to flow freely.
Peripheral arterial disease starts when fatty deposits start streaking the blood vessel walls. The fatty matter builds up. This causes slight injury to your blood vessel walls. In an attempt to heal itself, the cells release chemicals that make the walls stickier. Other substances floating through your bloodstream start sticking to the vessel walls, such as inflammatory cells, proteins and calcium. The fat and other substances combine to form a material called plaque or atherosclerosis. The plaque builds up and narrows the artery.
Over time, the inside of the arteries develop plaques of different sizes. Many of the plaque deposits are hard on the outside and soft and mushy on the inside. The hard surface can crack or tear, exposing the soft, fatty inside. When this happens, platelets (disc-shaped particles in the blood that aid clotting) come to the area, and blood clots form around the plaque. The artery narrows further. Symptoms occur.
The artery may become completely blocked by plaque or a blood clot that lodges in a narrowed artery. If this occurs, the tissue below the blockage is permanently damaged and may die (gangrene). This most often occurs in the toes and feet.
PAD in Women
Have you ever had to cut short a day of shopping or sightseeing because of severe leg pain? Maybe you’ve given up golf because you can no longer walk the course.
Pain or discomfort in the legs is a common symptom of a disease called peripheral arterial disease (PAD). Up to 8-12 million Americans have PAD. Peripheral arterial disease is atherosclerosis that develops in the arteries of the legs or, less commonly, the arms. Like atherosclerosis in the heart (coronary) arteries, PAD is caused by the accumulation of fatty plaque in the blood vessel walls. As plaque builds up, the blood vessels get narrower and narrower, until they become blocked. In the coronary arteries, atherosclerosis causes chest pain or a heart attack. In the legs, atherosclerosis can cause pain, weakness, or fatigue while walking.
The dangers of PAD extend well beyond difficulties in walking, and the consequences can be far worse than missing a shopping trip or golf game. Peripheral artery disease increases the risk of developing a non-healing sore of the legs or feet. In cases of severe PAD, these sores can develop into areas of dead tissue (gangrene) that ultimately require amputation of the foot or leg.
The effects of PAD can extend beyond the affected limb. The body’s circulatory system is interconnected. Patients with atherosclerosis of the legs commonly have atherosclerosis in other parts of the body. Therefore, it’s not surprising that patients with peripheral artery disease are at increased risk for having a heart attack, stroke, transient ischemic attack (“mini-stroke,”) or problems with the kidney (renal) arteries.
Who Gets PAD?
Although PAD is a different condition than coronary artery disease, the two are related. People who have one are likely to have the other: the National Institutes of Health estimates that a person with PAD has a six to seven times higher risk of coronary artery disease, heart attack, stroke or a transient ischemic attack than the general population; a person with heart disease has a 1 in 3 chance of having peripheral artery disease in the legs (1).
Not surprisingly, the two diseases also share some common risk factors. This is because these risk factors cause the same changes in arteries in the arms and legs as they do in the coronary arteries.
PAD risk factors include:
- Age over 50
- Smoking
- Diabetes
- High blood pressure
- High cholesterol
- Abdominal obesity
- Kidney disease (both a risk factor and a consequence of PAD)
Other risk factors for PAD include race – African Americans have about two times the risk for PAD as Caucasians or Asians – and a family history of heart disease or PAD.
Both woman and men are at risk for developing PAD.
As in coronary artery disease, many of these risk factors are out of your control. But, according to researchers at Cleveland Clinic (2), smoking is the single most important modifiable (changeable) risk factor for PAD and its complications. Smoking increases the risk for PAD by 400 percent and brings on PAD symptoms almost 10 years earlier. Compared with non-smokers of the same age, smokers with PAD are more likely to die of heart attack or stroke, have poorer results with heart bypass surgery procedures on the legs and are twice as likely to have a limb amputated.
Diabetes is another strong risk factor for PAD in women. When combined with other, common conditions related to diabetes such as heart disease, nerve problems in the legs and feet, visual problems, obesity and depression, adding PAD to the mix increases the likelihood that a diabetic woman will have serious mobility problems.
SYMPTOMS AND CAUSES
What are the symptoms of peripheral arterial disease?
PAD can build up over a lifetime, and the symptoms may not become obvious until later in life. For many people, the outward symptoms will not appear until the artery has narrowed by 60 percent or more.
The first noticeable symptom of PAD may be intermittent claudication -- leg discomfort, pain or cramping that develops with activity, is relieved with rest, and recurs upon resuming activity. The pain is often noticed in the calf, but may also be felt in the buttocks or thighs. Intermittent claudication symptoms may also include numbness, weakness, heaviness or fatigue in the leg muscles when walking that are relieved at rest. The pain can be severe enough to interfere with normal walking. This type of cyclical pain is caused by reduced blood flow to the leg muscles and goes away at rest because the muscles require less blood flow at rest.Other symptoms of advanced PAD may include:
- A burning or aching pain in the feet and toes while resting, especially at night while lying flat
- Cool skin in the feet
- Redness or other color changes of the skin
- Increased occurrence of infection
- Toe and foot sores that do not heal
Many people with PAD do not have any symptoms.
DIAGNOSIS AND TESTS
How is PAD detected?
Talk to your doctor if you are having symptoms of PAD so the cause of your symptoms can be identified and treatment can be initiated as soon as possible. Early detection of PAD is important so the right treatments can be provided before the disease becomes severe enough to lead to complications, such as heart attack or stroke.
A physical exam will be performed and your medical history and risk factors will be reviewed. Your doctor may order certain tests to help diagnose PAD and determine the severity of the disease.
- The ankle/brachial index (ABI) is a measurement of the blood pressure in the lower legs compared to the blood pressure in the arms. During this test, blood pressure cuffs are placed on the arms and legs. The cuffs are inflated, while a hand-held device (called a Doppler) is used to listen to the blood flow. The ABI screening helps evaluate the amount of blood flow to the legs and feet, which is decreased in a person with PAD. It is a highly accurate method for detecting PAD.
- A pulse volume recording (PVR) is a noninvasive test that measures the blood volume changes that occur in the legs. During this test, a blood pressure cuff is placed on the arm and multiple cuffs are placed on the legs. The cuffs are inflated slightly while the patient is lying down. As blood pulses through the arteries, the blood vessels expand, causing an increase or decrease in the volume of air within the cuff. A recording device displays these pulse volume changes as a waveform on a monitor. Blood pressures are measured before and after exercise on a treadmill and help define if the pain is due to PAD or other causes. The PVR test also helps locate the area of blockages in the legs.
- A vascular ultrasound is a noninvasive test used to examine blood circulation. During a vascular ultrasound, a transducer (small hand- held device) is placed on the skin over the artery to be examined. The transducer emits sound waves that bounce off the artery. These sound waves are recorded, and an image of the vessel is created and displayed on a monitor. This test may be used to detect a blockage in an artery.
MANAGEMENT AND TREATMENT
How is PAD treated?
Lifestyle changes, medications and interventional procedures are the treatments available for PAD.
Lifestyle Changes. Initial treatment of PAD includes making lifestyle changes to reduce your risk factors. Changes you can make to manage your condition include:
- Quit smoking. Ask your doctor about smoking cessation programs available in your community.
- Eat a balanced diet that is high in fiber and low in cholesterol, fat and sodium. Limit fat to 30 percent of your total daily calories. Saturated fat should account for no more than 7 percent of your total calories. Avoid trans fats including products made with partially-hydrogenated and hydrogenated vegetable oils. If you are overweight, losing weight will help you lower your total cholesterol and raise your HDL (good) cholesterol. A registered dietitian can help you make the right dietary changes.
- Exercise. Begin a regular exercise program, such as walking. Walking is very important and can aid the treatment of PAD. Patients who walk regularly can expect a marked improvement in the distance they are able to walk before experiencing leg pain. (See Walking Program Box)
- Manage other health conditions, such as high blood pressure, diabetes or high cholesterol.
- Practice good foot and skin care to prevent infection and reduce the risk of complications. (See Foot Care Guidelines Box)
Medications may be recommended to treat conditions such as high blood pressure (anti- hypertensive medications) or high cholesterol (statin medications).
An antiplatelet medication such as aspirin or clopidogrel (Plavix) may be prescribed to reduce the risk of heart attack and stroke.
Walking Program
Vascular Medicine and Preventive Cardiology and Rehabilitation offer a structured supervised walking program to help you succeed and maximize your exercise efforts. Please call 216.444.4420 or 800.223.2273 ext. 4420 to make an appointment.
Cilostazol (Pletal) may be prescribed to improve walking distance. This medication has been shown to help people with intermittent claudication exercise longer before they develop leg pain and to walk longer before they must stop because of the pain. However, not all patients are eligible to take this medication. Your doctor will tell you if you are eligible.
Interventional procedures. More advanced PAD can be treated with interventional procedures such as angioplasty (to widen or clear the blocked vessel), angioplasty with stent placement (to support the cleared vessel and keep it open), or atherectomy (to remove the blockage).
In some cases, surgical procedures such as peripheral artery bypass surgery may be performed to reroute blood flow around the blood vessel blockage.
New therapies are currently being researched. Please ask your doctor if any other treatment options are available for you.
If any of these procedures are recommended, your health care team will give you more information about the procedures so you will know what to expect.
Can PAD be cured?
There is no cure for PAD. Quitting smoking, exercising regularly, limiting fat and following a healthy diet, and managing your risk factors — such as diabetes, high cholesterol and high blood pressure — can help to reduce the progression of the disease.
Foot Care Guidelines
Every day, examine your legs as well as the tops and bottoms of your feet and the areas between your toes. Look for any blisters, cuts, cracks, scratches or other sores. Also check for redness, increased warmth, ingrown toenails, corns and calluses. Use a mirror to view the leg or foot if necessary, or have a family member look at the area for you.
Once or twice a day, apply a moisturizing cream or lotion to your legs and soles and top of your feet to prevent dry skin and cracking. Do not apply lotion between your toes or on areas where there is an open sore or cut. If the skin is extremely dry, use the moisturizing cream more often. Care for your toenails regularly. Cut your toenails after bathing, when they are soft. Cut toenails straight across and smooth with a nail file.
If you have diabetes, it is important to see a podiatrist.
Do not self-treat corns, calluses or other foot problems. Go to a podiatrist to treat these conditions.
Don't wait to treat a minor foot or skin problem. Follow your doctor's guidelines.
Other tests may include angiography, CT scan or MRI.
During angiography (also called arteriography), contrast material (dye) is injected into the blood vessels being examined, and X-ray pictures of the inside of the blood vessels are produced to evaluate blood flow and detect possible blockages.
A CT scan is a technique in which multiple X-rays are taken from different angles in a very short period of time. The images are collected by a computer and cross-sectional “slices” of the blood vessel are shown on the monitor.
MRI uses powerful magnets to create images of internal organs and blood vessels.
Taking Control of Peripheral Arterial Disease
Despite the prevalence of PAD, it is surprisingly underdiagnosed and undertreated (3). The good news is that, although PAD is a serious condition with potentially serious consequences, it is treatable. Like most health conditions, PAD is more treatable when it is detected early.Being aware that you have risk factors for PAD may motivate you to take action to prevent PAD from developing. The same advice for maintaining a healthy heart applies to maintaining healthy circulation overall:
- Manage your weight
- Eat a low fat, low sugar diet that includes at least five servings of fresh fruits and vegetables every day
- Don’t smoke.
- With your doctor’s approval, exercise, doing an activity you enjoy, for at least 30 minutes a day on most days of the week.
If you have heart disease, you should discuss your risk factors for PAD with your doctor and report any symptoms you are having such as pain, weakness or numbness in the legs. Your doctor may order a simple test, known as the ankle-brachial index (ABI), to diagnose PAD The ABI test involves measuring the blood pressures in the arms and the legs using a hand-held Doppler device.
If you already have mild PAD, your doctor may prescribe exercise therapy, dietary changes, smoking cessation and medication. Common medications prescribed for atherosclerosis and PAD include anti-platelet agents (such as aspirin or clopidogrel) and cholesterol lowering medications (“statins”). The best things that you can do for yourself in this situation are to quit smoking, control your high blood pressure, take your medications, and manage your diabetes.
It is also very important that patients with PAD take especially good care of the feet to prevent non-healing sores. Important components of foot care for patients with PAD include: wearing comfortable, appropriately fitting shoes; inspecting the feet regularly for sores; keeping the feet clean and well moisturized; and, taking regular care of the toe nails. In some cases, a patient with PAD is referred to a podiatrist for specialized foot care.
Other Treatments for Peripheral Arterial Disease
More advanced PAD that is causing severe pain and limited mobility may require endovascular (i.e., minimally invasive) or surgical treatment. Some of the same treatments that are used for heart disease are also used for treating PAD.
Balloon angioplasty:
In this procedure, a miniature balloon is passed through a catheter into the arteries. As the balloon is expanded inside the artery, it pushes against the plaque and opens up the artery.
Stents:
These are tiny metal support coils that are inserted into the arteries. Once they are in place, stents expand against the inner blood vessel wall to support it and hold it open. Stents can be placed through a small opening using catheters (long, thin tubes) without major surgery.
Bypass surgery:
Similar to heart bypass, a surgeon uses a section of the patient's healthy vein or a synthetic replacement to create a bypass around the blocked area in the leg artery. This is usually reserved for the most severe PAD.
With early diagnosis, lifestyle changes and treatment, you can stop PAD from getting worse. In fact, some studies have shown that symptoms due to PAD can be reversed with exercise combined with careful control of cholesterol and blood pressure. If you think you are at risk for PAD or may already have the disease, talk to your primary care doctor or cardiologist so that you can get started on a prevention or treatment program as soon as possible. With proper diagnosis and treatment, you can still enjoy the good things in life - like shopping, sightseeing and golf!
For questions or more information about PAD, call the Miller Family Heart, Vascular & Thoracic Institute Resource and Information Center Nurse at 216.445.9288 or toll-free 866.289.6911. For an appointment with a Cleveland Clinic women’s heart or vascular specialist, call toll-free 800.223.1696 or locally, 216.444.9343.
PREVENTION
Know the Warning Signs of Peripheral Artery Disease (PAD)
One of the Deadliest Diseases You’ve Never Heard Of
More than 8 million Americans suffer from peripheral arterial disease, or PAD. Just as a heart attack is caused by a blocked artery in the heart, PAD is the same kind of blockage – only it takes place in the arm, leg or other part of the body.
PAD is a leading cause for amputation, and puts you at risk for heart attack, stroke and death. It can build up over a lifetime, and the symptoms may not become obvious until later in life.
The first noticeable symptom of PAD may be a painful cramping in the calf, thigh or buttocks that occurs regularly when you walk or move, but that goes away when you’re at rest. This is called intermittent claudication. The pain can be severe enough to limit your ability to participate in activities you enjoy, such as golfing or chasing after grandchildren.
Other symptoms of advanced PAD include:
- Burning or aching pain in the feet and toes while resting (especially at night while lying flat)
- Cool skin in the feet
- Redness or color changes in the skin
- Toe and foot sores that do not heal.
But fully half of people who have PAD experience no symptoms at all. That’s one of the reasons it’s so dangerous.
What are the risk factors for PAD?
An individual is at risk for developing PAD when one or more of these risk factors are present:
- Smoking
- Diabetes
- Age: In the United States, people aged 50 and older have an increased risk for PAD
- Race: African Americans have a two-fold higher risk of developing PAD compared to other groups
- History of heart or blood vessel disease: A personal or family history of heart or blood vessel disease may be an indicator for PAD
- High blood pressure (hypertension)
- High cholesterol (hyperlipidemia)
RESOURCES
Doctors vary in quality due to differences in training and experience; hospitals differ in the number of services available. The more complex your medical problem, the greater these differences in quality become and the more they matter.
Clearly, the doctor and hospital that you choose for complex, specialized medical care will have a direct impact on how well you do. To help you make this choice, please review our Miller Family Heart, Vascular & Thoracic Institute Outcomes.
Cleveland Clinic Heart, Vascular & Thoracic Institute Vascular Medicine Specialists and Surgeons
Choosing a doctor to treat your vascular disease depends on where you are in your diagnosis and treatment. The following Heart, Vascular & Thoracic Institute Sections and Departments treat patients with all types of vascular disease, including blood clotting disorders:
Section of Vascular Medicine: for evaluation, medical management or interventional procedures to treat vascular disease. In addition, the Non-Invasive Laboratory includes state-of-the art computerized imaging equipment to assist in diagnosing vascular disease, without added discomfort to the patient. Call Vascular Medicine Appointments, toll-free 800-223-2273, extension 44420 or request an appointment online.
Department of Vascular Surgery: surgery evaluation for surgical treatment of vascular disease, including aorta, peripheral artery, and venous disease. Call Vascular Surgery Appointments, toll-free 800-223-2273, extension 44508 or request an appointment online.
You may also use our MyConsult second opinion consultation using the Internet.
The Heart, Vascular & Thoracic Institute also has specialized centers and clinics to treat certain populations of patients:
Learn more about experts who specialize in the diagnosis and treatment of vascular and arterial disease.

0Comments